
Chronic Obstructive Pulmonary Disease (COPD), commonly associated with smokers, is a significant health concern that impacts millions globally. This article aims to shed light on the intricacies of COPD, from its causes and symptoms to its management and prevention.
Whether you’re a patient, a caregiver, or someone keen on understanding this respiratory ailment, our comprehensive guide provides insights that are both informative and actionable.
Join me as we explore the multifaceted world of COPD and the steps we can take towards a healthier future.
Section 1: Introduction to COPD (Smoker’s Lung) and its Main Types
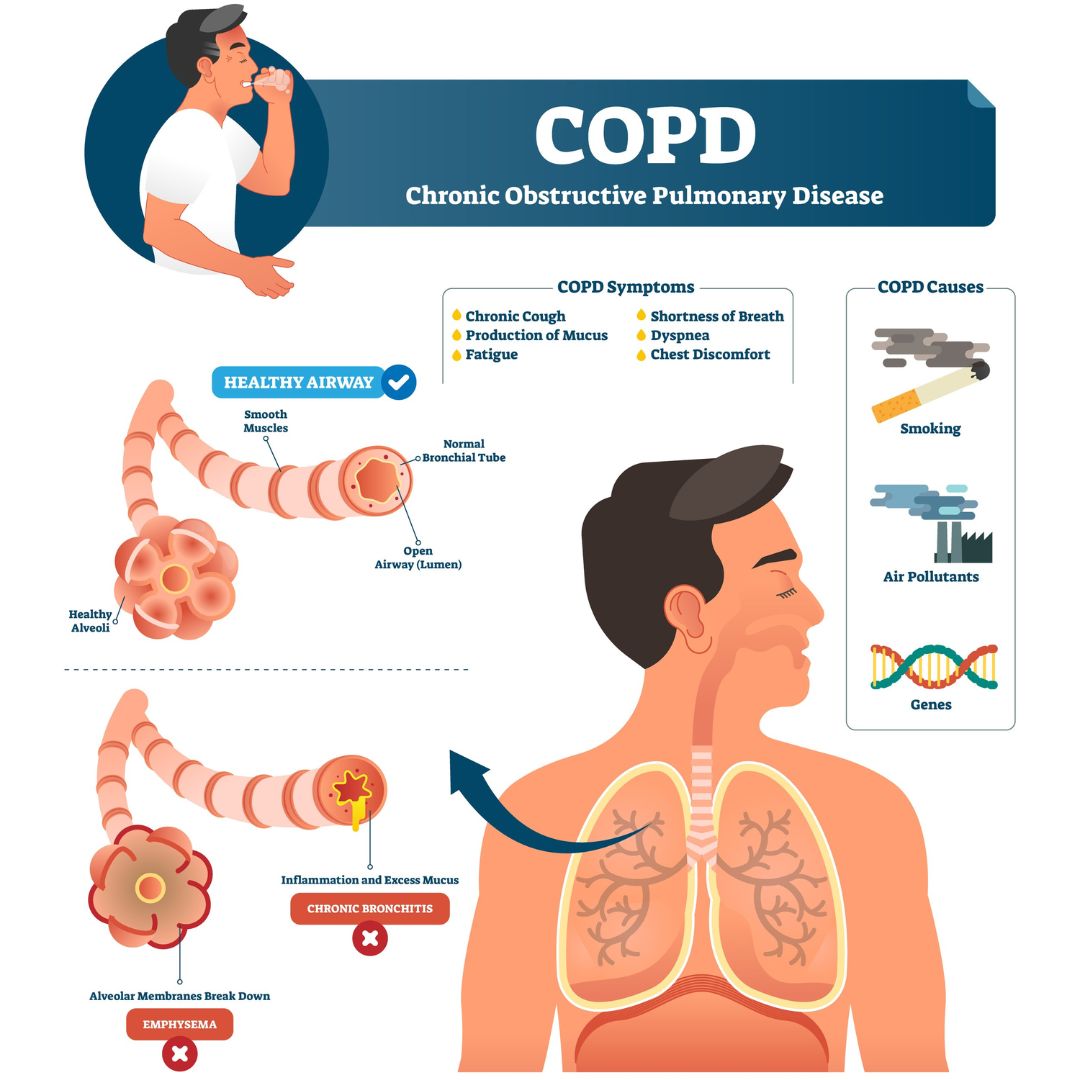
Chronic Obstructive Pulmonary Disease, better known as COPD, is a progressive lung disease that hampers breathing. It’s a condition that many in Malaysia and around the world face, especially those with a history of prolonged smoking. At its core, COPD is the result of obstructed airflow from the lungs, leading to difficulty in breathing and reduced oxygen levels in the body.
Often termed “Smoker’s Lungs”, COPD is most commonly found among individuals who have been regular smokers for a significant period. To give you an idea, imagine someone who has smoked more than one pack a day for over 20 years. The damage from the smoke and harmful chemicals leads to inflammation and eventually results in COPD.
Let’s discover the two primary types of COPD:
- Chronic Bronchitis Type: This variant of COPD is characterized by a long-term cough with mucus. People with this condition often experience swollen, inflamed bronchial tubes that produce a lot of mucus. As a result, a persistent cough develops. Due to its characteristics, it’s sometimes termed “Blue Bloaters“.
- Emphysema Type: This type mainly affects the air sacs in the lungs. Over time, these air sacs get damaged and lose their stretchiness. This makes it hard for people to breathe out fully and get fresh air in. Because of the way it manifests, it’s often called “Pink Puffers“.
Understanding the types of COPD is essential for effective treatment and management. In the next section, we’ll uncover the various symptoms of COPD, helping you recognize the signs early for better intervention.
Section 2: Symptoms of COPD
COPD, while commonly linked to smoking, can manifest differently in patients. But one thing remains consistent: the challenges and difficulties they face in their daily lives due to the symptoms. Let’s delve into the typical symptoms that COPD patients often describe:
- Difficulty Breathing: The most commonly reported symptom is a difficulty in breathing. Patients often describe this as a feeling of shortness of breath. This becomes particularly noticeable during physical activities. Simple tasks, like walking or climbing stairs, can become daunting challenges. Imagine being in a rush and feeling a significant breathlessness; that’s what many COPD patients experience.
- Panting Episodes: Often, after excessive physical exertion, patients report episodes of panting. This isn’t the usual out-of-breath feeling after a run but a more severe form that can be quite distressing.
- Chronic Cough: A persistent cough, especially prevalent in the mornings, is another sign of COPD. This isn’t your typical seasonal cough but a prolonged one that can cause discomfort.
- Phlegm Production: Along with the chronic cough, patients may produce phlegm. While it’s usually whitish, the color can change to green or yellow, especially during infections.
Understanding these symptoms is crucial, not just for diagnosis but also for managing the condition effectively.
In the following section, we’ll hear from a patient directly. Their story will shed light on the real-world challenges and experiences of living with COPD.
Section 3: Patient Story – the Severity of COPD Exacerbations
During my years of practice, I encountered a particularly memorable patient. This gentleman, in his 50s, had been a chronic smoker from his early twenties. His commitment to the habit, which involved consuming one to two packs daily, was unwavering until he faced a health crisis. A severe lung infection led to his hospital admission, and the severity of his condition was such that he required immediate care in the Intensive Care Unit (ICU). Unfortunately, his health challenges did not end there. During his hospital stay, he also suffered a heart attack. Such cardiac complications are, sadly, not uncommon among COPD patients. The inflammation from COPD has a ripple effect, potentially impacting even the heart muscles.
With a combination of nebulizer treatments, antibiotics, and specialized COPD care, he began his recovery process. This deeply challenging hospital experience became a catalyst for change in his life. Recognizing the grave consequences of his smoking habit, he made the pivotal decision to quit. This choice, bolstered by regular inhaler treatments, paved the way for a renewed chapter in his life. After quitting smoking, he remained free from further COPD exacerbations and managed to lead a fulfilling life.
In the next section, we’ll delve deeper into the intricate relationship between COPD and heart issues, shedding light on the interconnectedness of our body systems.
Section 4: Understanding a COPD Exacerbation or ‘Lung Attack’
Chronic Obstructive Pulmonary Disease (COPD) is generally a stable condition for many patients. However, there are instances when the symptoms suddenly worsen, becoming intense and more severe. This acute flare-up is termed as a COPD exacerbation or colloquially known as a ‘lung attack.’
Much like how a heart attack signifies a sudden and critical heart condition, a ‘lung attack’ indicates a crucial turning point in a COPD patient’s health. It’s a severe escalation of their usual COPD symptoms, requiring immediate medical attention. This phase is distinctly different from the stable periods that a COPD patient typically experiences.
Several factors can trigger these exacerbations:
- Infections: Even common infections like the flu or cold can set off an exacerbation in COPD patients. More severe respiratory infections, such as pneumonia, are also potential triggers.
- Weather and Climate: Surprisingly, the weather plays a role too. Extreme cold, a sudden downpour, or intense heat can precipitate a ‘lung attack.’ Rapid changes in weather conditions can be particularly problematic for COPD patients.
- Environmental Pollutants: Exposure to polluted environments, smoke, or dust doesn’t just harm healthy lungs. For those with COPD, these irritants can be the tipping point, leading to an exacerbation.
Recognizing and understanding the nature and triggers of a ‘lung attack’ is crucial. It empowers patients and caregivers to be vigilant, enabling timely interventions and management of the condition.
In the next section, we’ll look at what are the symptoms associated with COPD exacerbations.
Section 5: Symptoms of COPD Lung Attacks
COPD exacerbations, commonly known as lung attacks, present a set of symptoms that are more intense than the usual manifestations of the disease. Recognizing these signs is crucial for patients and caregivers, as it can signal the need for immediate medical attention.
Here are the primary symptoms of a COPD lung attack:
- Intensified Cough: During a lung attack, patients experience a more severe and frequent cough than usual.
- Change in Phlegm: While typical COPD phlegm may be yellow or whitish, during an exacerbation, it can change in color and consistency. It might turn yellowish, greenish, or even purulent. Additionally, there’s an increase in the volume and frequency of the phlegm.
- Sleep Disturbances: A persistent cough and difficulty breathing during a lung attack often disrupt sleep. This continuous disturbance leads to fatigue and lethargy during the day, affecting a patient’s overall productivity.
- Breathing Difficulties: Shortness of breath becomes more pronounced, making even simple activities challenging.
- Audible Wheezing: An acute exacerbation might also be accompanied by a wheezing sound, which can be heard when the patient breathes.
- Fatigue: Due to disrupted sleep and the body’s constant effort to breathe, patients often feel exceptionally tired and drained.
Understanding these symptoms can help in timely intervention and better management of the disease during its critical phases.
In the next section, we’ll explore the changes that occur in the lungs during a lung attack, offering insights into the physiological responses of the body.
Section 6: What Happens in the Lungs During a Lung Attack?
For many, the term “lung attack” might seem abstract, but for a patient with COPD, it’s a distressing reality. When someone with COPD or smokers’ lungs undergoes an acute exacerbation, several physiological processes occur in the lungs:
- Excessive Inflammation: The lungs experience heightened inflammation, leading to the release of numerous inflammatory mediators into the bloodstream.
- Bronchoconstriction: A typical airway is open, allowing air to flow in and out effortlessly. However, during a lung attack, bronchoconstriction occurs. This means that the airways constrict or narrow down, making breathing challenging. The normally open airways become significantly narrowed, causing the hallmark symptom of shortness of breath.
- Hypersecretions: Alongside the constriction, the airways’ glands produce excessive secretions. This overproduction results in a buildup of phlegm and other secretions in the airways.
- Persistent Cough: As a result of these hypersecretions, patients experience a continuous cough, often accompanied by whitish or yellowish phlegm.
These physiological changes provide a glimpse into the challenges COPD patients face during an exacerbation. The narrowing of airways, combined with inflammation and excess secretions, creates the perfect storm, making breathing a laborious task.
In the next section, we’ll explore the differences between COPD and asthma, two respiratory conditions that, while sharing some similarities, have distinct characteristics and management approaches.
Section 7: Differences & Similarities Between COPD and Asthma
Both COPD and asthma are respiratory conditions, and due to their overlapping symptoms, they can often be confused for one another. Here’s a closer look at the similarities and key differences between the two:
Similarities:
- Symptoms Overlap: Both COPD and asthma patients experience difficulty breathing, panting, shortness of breath, and coughing. This overlap in symptoms can sometimes lead to misdiagnosis.
Differences:
- Nature of Cough:
- Asthma: Asthmatic patients often have a dry cough.
- COPD: Those with COPD tend to have a productive cough, meaning they cough up phlegm. This phlegm is typically whitish in color.
- Genetic Factors:
- Asthma: Asthma often runs in families. Many asthmatic patients have a significant family history, with siblings or parents also suffering from the condition.
- COPD: The primary factor leading to COPD isn’t genetic but environmental. A significant history of smoking is the most common cause behind the development of COPD.
- Primary Cause:
- Asthma: Often linked to genetic predispositions and environmental triggers.
- COPD: Predominantly caused by prolonged exposure to lung irritants, with smoking being the most common culprit.
Understanding these distinctions is crucial for accurate diagnosis and treatment. Proper management and interventions can significantly improve the quality of life for patients, irrespective of whether they have COPD or asthma.
In the next section, we’ll further explore the age at which a patient might develop either COPD or asthma, shedding light on the factors that contribute to each disease.
Section 8: Age of Onset – COPD vs. Asthma
While both COPD and asthma are respiratory conditions, the age at which individuals might start showing symptoms can vary significantly between the two. This difference in the onset of symptoms can provide valuable insights during diagnosis:
- Asthma:
- Onset: Asthma symptoms typically begin in early childhood. Many children who are diagnosed with asthma experience a range of symptoms.
- Progression: For a significant number of these children, symptoms tend to resolve or decrease as they grow older, especially as their immune systems mature.
- Associated Conditions: Asthmatic patients often have associated allergic conditions. These can include allergic rhinitis (affecting the nose) and conditions affecting the digestive tract like reflux esophagitis or gastritis.
- COPD:
- Onset: In contrast, COPD symptoms usually manifest later in life, typically around the ages of 40 to 50.
- Progression: The disease’s progression is closely linked to smoking. The condition can continue to worsen if the individual continues to smoke. However, upon quitting smoking, the progression of COPD tends to stabilize.
- Associated Conditions: Unlike asthmatics, those with COPD typically don’t have associated allergic conditions.
By understanding these distinctions, healthcare professionals can make more informed decisions about potential diagnoses and treatment plans.
In the next section, we’ll dive into the intricacies of diagnosing COPD, highlighting the steps and considerations involved in the process.
Section 9: Diagnosing COPD
Diagnosing Chronic Obstructive Pulmonary Disease (COPD), also referred to as smoker’s lung, involves a comprehensive approach. This process is crucial to ensure accurate identification and effective management of the condition. Here’s how medical professionals typically diagnose COPD:
- Medical History:
- Smoking History: One of the first factors explored is whether the patient has a history of smoking. Smokers are more predisposed to develop COPD.
- Age of Symptom Onset: Typically, symptoms of COPD begin to manifest around the age of 40 or later.
- Physical Examination:
- Lung Structure: One key indicator is the appearance of the lungs. Those with COPD may have barrel-shaped lungs.
- Breathing Patterns: Particularly for the ‘pink puffer’ type of COPD, patients often display a distinctive breathing pattern. They breathe primarily through their mouths, appearing to puff as they do so. This puffing phenomenon, especially evident during the exhalation phase, is the body’s way of controlling breathing.
- Further Testing:
- Once the initial history and physical examination point towards COPD, further testing is required to confirm the diagnosis. One such crucial test is spirometry.
In the next section, we’ll explore the role of spirometry testing in diagnosing COPD, understanding its significance, and how it aids in the evaluation of lung function.
Section 10: The Role of Spirometry in COPD Diagnosis
Spirometry plays a pivotal role in diagnosing respiratory conditions, especially when differentiating between COPD and asthma. Here’s why spirometry is considered the gold standard for such diagnoses:
- Differentiating COPD from Asthma:
- Reversibility Test: The primary distinction between asthma and COPD using spirometry revolves around the concept of reversibility. After being administered an inhaler during the spirometry test, asthmatic patients typically show a significant improvement in lung function. This indicates that the airway obstruction they experience is reversible.
- Permanent Damage in COPD: In contrast, COPD patients have permanent lung damage, often resulting from prolonged smoking. Despite being given a nebulizer or inhaler during the test, their lung function does not show the same degree of improvement as seen in asthma patients.
- Identifying the Type of Lung Problem:
- Obstructive vs. Restrictive: Spirometry can help medical professionals determine if a patient has an obstructive or restrictive lung function issue. This distinction is vital in diagnosing COPD, asthma, or other lung conditions like interstitial lung disease, which involves lung scarring.
- Deciding the Course of Treatment: The results from the spirometry test are crucial in guiding the treatment plan. It provides clarity on the type and extent of lung damage, enabling physicians to tailor the treatment accordingly.
In the next section, we’ll discover how X-ray examinations further aid in the diagnostic process, offering insights into the structural changes in the lungs.
Section 11: The Significance of X-ray in COPD Diagnosis
When diagnosing COPD, a chest X-ray serves as a valuable tool, providing physicians with a visual representation of the lungs and surrounding structures. Here’s what medical professionals typically observe in an X-ray of a COPD patient:
- Hyperinflated Lungs:
- COPD patients often have lungs that appear hyperinflated, meaning they are enlarged compared to those in healthy individuals. This hyperinflation is a hallmark sign of COPD and can be clearly observed in X-ray images.
- Tubular Heart:
- Due to the enlarged lungs, the heart can appear compressed or smaller than usual, sometimes taking on a tubular shape. This characteristic appearance is another indicator of COPD.
- Flattened Diaphragm:
- The diaphragm, a primary muscle responsible for breathing, can appear flattened in COPD patients. This change is due to the hyperinflated lungs pushing down on the diaphragm.
- Evidence of Infections:
- An X-ray can also help identify other conditions or complications associated with COPD. For instance, white patches on the lungs might indicate pneumonia, an infection that COPD patients are more susceptible to.
- Additionally, the presence of air trapped in the space between the lung and chest wall, known as pneumothorax, can also be detected. This condition is particularly common in COPD patients and can be life-threatening if not addressed promptly.
X-rays offer invaluable insights into the structural changes in the lungs and surrounding areas, enabling more accurate diagnosis and tailored treatment plans.
In the next section, we’ll explore how CT scans provide a more detailed view of the respiratory system, enhancing our understanding of lung conditions.
Section 12: Role of CT Scan in COPD Diagnosis
One of the advanced diagnostic tools at our disposal for COPD is the CT scan of the lungs. This imaging technique offers a detailed look into the lungs, revealing nuances that might be missed with other tests. Here’s how a CT scan aids in diagnosing and understanding the severity of COPD:
- Type of COPD:
- A CT scan can help determine the specific type of COPD a patient has, be it the chronic bronchitis type or the emphysematous type.
- Extent of Emphysema:
- The scan reveals the type of emphysematous changes present in the lungs.
- It allows for an assessment of the percentage of the lung affected by these changes, giving a clear picture of the disease’s extent.
- Location of the Problem:
- With a CT scan, medical professionals can pinpoint where the most significant pathological issues related to emphysema are located. It could be in the upper or lower parts of the lungs, or it might be localized to one side or involve both lungs.
- Informing Treatment Decisions:
- Understanding the severity and location of COPD via CT scans allows doctors to tailor treatment plans more effectively.
- By knowing the percentage of lung involvement, decisions can be made regarding the most suitable treatment, from inhalers to interventional approaches.
CT scans, therefore, play a pivotal role in not only diagnosing COPD but also in determining its severity and guiding the treatment strategy.
In the next section, we’ll discuss the role of antibiotics in the management of COPD and when they become essential in the treatment plan.
Section 13: Role of Antibiotics in COPD Treatment
Antibiotics are a vital component in the treatment toolkit for COPD, especially when patients experience complications like acute lung infections. Here’s how antibiotics play a role in managing COPD:
- Combatting Infections:
- In COPD patients, acute infections such as pneumonia or bronchitis can exacerbate their symptoms. Antibiotics are essential in these scenarios to eliminate pathogens, germs, and bacteria, helping to alleviate the infection.
- Type of Antibiotic Administration:
- The mode of administering antibiotics largely depends on the severity of the patient’s condition.
- Severe Cases: For critically ill patients, especially those in ICU, powerful, high-end antibiotic injections are needed to rapidly stabilize and counteract the infection.
- Milder Cases: For stable patients who don’t require supplemental oxygen and are treated in a standard hospital ward, antibiotic tablets might be sufficient. While injections can still be used, they might be of a less potent variety.
- The mode of administering antibiotics largely depends on the severity of the patient’s condition.
- Significance in Treatment:
- Antibiotics are crucial when a COPD patient develops an acute lung infection. Swift and effective treatment can prevent complications and ensure a quicker recovery.
In the next section, we’ll discuss the significance of monitoring and controlling blood pressure in COPD patients and its impact on their overall health.
Section 14: Importance of Blood Pressure Control in COPD
Managing blood pressure is crucial in the comprehensive care of COPD patients. Here’s why it’s an essential aspect of treatment:
- Low Blood Pressure in Severe Cases:
- Particularly in severely ill COPD patients requiring ICU care, blood pressure often tends to be on the lower side. This situation necessitates medical intervention to stabilize the blood pressure.
- Impact on the Elderly:
- Elderly individuals with COPD, when faced with a severe infection, can experience weakened heart function. This, in turn, can lead to a drop in blood pressure. In such scenarios, medical support becomes critical to maintain adequate blood pressure levels and ensure proper heart function.
- Inotropic Support:
- To bolster the heart and maintain blood pressure, inotropic support is administered. This treatment involves the use of specific medications:
- Dobutamine infusion
- Dopamine
- Noradrenaline
- The choice of medication is based on the nature of the infection and the severity of the COPD exacerbation.
- To bolster the heart and maintain blood pressure, inotropic support is administered. This treatment involves the use of specific medications:
- Specialized Care:
- Patients requiring inotropic support typically need ICU care. Their treatment is often co-managed by an anesthetist specialist to ensure the best possible outcomes.
In the next section, we’ll explore the use of IV drips in the treatment and management of COPD and how they contribute to the patient’s recovery process.
Section 15: The Importance of IV Drip in COPD Management
Hydration is crucial for everyone, but for COPD patients experiencing an acute exacerbation or lung attacks, maintaining hydration becomes even more critical. Here’s why an Intravenous (IV) drip is often essential for these patients:
- Breathing Difficulties & Nutritional Challenges:
- When COPD patients suffer from acute exacerbations, they struggle to breathe. This difficulty can interfere with their ability to eat and drink without choking or coughing. Their rapid breathing rate often prevents them from consuming food or liquids comfortably.
- Increased Breathing Rate:
- A normal breathing rate ranges from 12 to 18 breaths per minute. However, for COPD patients during an exacerbation, this can skyrocket to 40 or even 50 breaths per minute. This accelerated rate further compounds their ability to consume food or drink.
- Ensuring Hydration & Nutrition:
- Given these challenges, it becomes paramount to ensure COPD patients remain hydrated and receive the necessary nutrients. This is where the IV drip plays a vital role. By administering fluids directly into the bloodstream, it guarantees that patients stay hydrated and nourished, even if they can’t eat or drink traditionally.
- Supporting Recovery:
- Proper hydration and nutrition are foundational for recovery. By providing these essentials through an IV drip, medical professionals ensure that COPD patients have the support they need to heal and regain strength.
In the next section, we’ll discuss nebulisation support and its role in aiding COPD patients, especially during acute episodes.
Section 16: Nebulization Support in COPD Management
Nebulization is a vital component in the comprehensive treatment of COPD. It’s a method commonly associated with asthma, but it’s equally crucial for COPD patients. Here’s how nebulization support benefits COPD patients:
- Opening Narrowed Airways:
- The primary purpose of nebulization therapy is to open up the constricted areas in the lungs that are characteristic of COPD patients. The mist from the nebulizer delivers medication directly to the lungs, helping to widen these narrowed passages.
- Frequency Based on Severity:
- The frequency of nebulization treatments varies depending on the severity of the COPD exacerbation.
- Very Ill Patients: In extreme cases, patients might require nebulization every hour to ensure their airways remain open.
- Stabilizing Patients: As the patient starts to show signs of improvement, the frequency of nebulization can be reduced. From hourly sessions, it can be decreased to every two hours, and then progressively to every four, six, or eight hours as the patient’s condition stabilizes.
- The frequency of nebulization treatments varies depending on the severity of the COPD exacerbation.
- Aiding Recovery:
- Regular and timely nebulization treatments play a crucial role in the patient’s recovery process. It ensures that the airways remain open, reducing the risk of complications and helping the patient breathe more comfortably.
In the next section, we’ll explore the role of Non-Invasive Ventilation (NIV) in COPD management and how it aids patients, especially during acute exacerbations.
Section 17: Non-Invasive Ventilation (NIV) in COPD Management
When dealing with severe cases of COPD, especially when standard oxygen support doesn’t yield the desired improvement, Non-Invasive Ventilation (NIV) becomes a critical treatment option. Here’s what you need to know about NIV:
- Why NIV?:
- NIV is essential when a COPD patient is too weak to breathe on their own. It provides an added layer of support to ensure the patient receives adequate oxygen and maintains proper respiratory function.
- Types of NIV:
- Different types of non-invasive ventilatory support are available based on the patient’s specific needs:
- BiPAP (Bilevel Positive Airway Pressure): Provides varying levels of pressure to assist with inhalation and exhalation.
- CPAP (Continuous Positive Airway Pressure): Offers constant pressure to keep the airways open.
- High Flow Nasal Cannula: Delivers a high flow of warm, humidified oxygen through a nasal cannula.
- Different types of non-invasive ventilatory support are available based on the patient’s specific needs:
- Mechanism:
- These devices work by providing added pressure, assisting in opening up the airways, and ensuring the COPD patient receives both the necessary oxygen and pressure support. This assistance is crucial for the patient to breathe efficiently and recover from their condition.
- Aiding Recovery:
- With the support of NIV, patients have a better chance of navigating their illness, ensuring they receive the oxygen they need, and reducing the risk of complications.
In the next section, we’ll delve into the importance of carefully measured oxygen support for COPD patients and how it’s crucial for their well-being.
Section 18: The Precision of Oxygen Support in COPD Management
Managing COPD requires a balance of treatments, and oxygen support is a key component. However, it’s not as simple as just providing oxygen. The process needs precision and careful monitoring. Let’s explore why:
- Initial Assessment:
- Treating a COPD patient begins with assessing the basic lifelines: airway, breathing, and circulation, often referred to as A, B, C.
- It’s crucial to determine whether the patient’s airway is open, if they can breathe independently, and if they require supplemental oxygen or additional ventilation support.
- Measuring Oxygen Levels:
- Once the initial assessment is complete, it’s imperative to measure the patient’s oxygen level. A low level indicates a need for supplemental oxygen.
- Precision is Key:
- While oxygen is essential, it’s a delicate balance for COPD patients. Providing too much oxygen can exacerbate their condition.
- Typically, care starts with a nasal prong delivering oxygen at three litres per minute. This delivery method is less intrusive and allows for consistent monitoring.
- Continuous Monitoring:
- After initiating oxygen support, regular checks are necessary to gauge whether the patient is improving or if adjustments are needed.
- Why Caution?:
- Excessive oxygen can lead to complications for COPD patients. It’s a condition where precision is paramount, ensuring patients get the support they need without causing additional issues.
In the next section, we’ll discuss the role of steroids in treating COPD and how they contribute to the overall management strategy.
Section 19: The Role of Steroids in COPD Management
When dealing with severe cases of COPD, especially during acute exacerbations, steroids play a crucial role in treatment. Here’s a breakdown of how steroids aid in managing COPD:
- Immediate Relief:
- Steroid injections, such as hydrocortisone, can provide rapid relief for critically ill COPD patients, especially those in the ICU.
- Within just 20 to 30 minutes of administration, these steroids can start to combat the inflammation causing distress.
- How Steroids Work:
- Steroids work by reducing the inflammation in the lungs. This inflammation is a primary cause of the symptoms experienced during a COPD exacerbation.
- By controlling the inflammation, steroids help to open up the airways and relax the constricted muscles, allowing for improved airflow and reduced symptoms.
- Dosage and Frequency:
- An initial ‘stat’ dose of the steroid is given immediately for quick relief.
- Subsequent doses are administered regularly, often three times a day, to maintain the anti-inflammatory effect and keep the patient stable.
- Why Steroids?:
- During a COPD exacerbation, significant inflammation occurs. This inflammation can lead to narrowed airways and muscle constriction, both of which make breathing difficult.
- Steroids act swiftly to suppress this inflammation, providing relief and improving the patient’s condition.
In our next section, we’ll share a patient story that highlights the complexities of COPD and how an exacerbation led to a heart attack, emphasizing the interconnectedness of our body’s systems.
Section 20: Patient Story – COPD Exacerbation and Heart Attack
Let me recount a story of a patient that demonstrates the intricate connections within our body and the potential complications of COPD.
A gentleman in his 50s, a chronic smoker since the age of 20, came under my care. His smoking habit was intensive, consuming one to two packs daily. This lifestyle led him to develop COPD, commonly referred to as smoker’s lung.
One fateful day, he was admitted to the hospital due to a severe lung infection. The situation was dire, and he needed immediate intensive care in the ICU. After some time, we managed to stabilize him enough for a transfer to the general ward. However, the complexities of his health didn’t end there. During his hospital stay, he suffered a heart attack.
It’s worth noting that many COPD patients are at risk of heart-related issues. The inflammation they experience in the airways can spread throughout the body. When it affects the heart muscles, the likelihood of a heart attack increases.
Thankfully, with the right treatment – a combination of a nebulizer, antibiotics, and other COPD-specific treatments – he began to recover. The traumatic experience in the hospital, combined with the heart attack, served as a wake-up call for him. He decided to quit smoking, a significant step in preventing further COPD exacerbations. With the support of proper inhaler treatment and lifestyle changes, he now leads a normal life.
In the next section, we’ll explore the benefits and methods of pulmonary rehabilitation, a vital component in the comprehensive management of COPD.
Section 21: Pulmonary Rehabilitation for COPD Management
Pulmonary rehabilitation plays a pivotal role in managing COPD. When patients are admitted due to COPD exacerbations or lung attacks, introducing them to pulmonary rehabilitation can significantly aid their recovery process.
What does pulmonary rehabilitation involve?
- Deep Breathing Technique: This technique promotes better lung function by teaching patients how to take deep, intentional breaths. It can help improve lung capacity and oxygen exchange, making it easier for patients to breathe.
- Incentive Spirometry Technique: This method uses a device to help patients improve the function of their lungs. It encourages a slow and deep breath, which can aid in opening up the airways and improve lung volume.
- Upper and Lower Limb Muscle Strengthening Exercise: COPD can often lead to muscle weakness, especially in the limbs. By incorporating specific exercises, patients can strengthen these muscles, making daily activities easier and improving overall quality of life.
In my practice, I often collaborate with physiotherapists. They possess the expertise to teach chest physiotherapy and other rehabilitation techniques that are beneficial for COPD patients. If you or your loved ones suffer from COPD, I strongly recommend liaising with a physiotherapist to explore the benefits of pulmonary rehab. It’s not just about treating the lungs; it’s about improving the overall well-being and lifestyle of those with COPD.
Stay with us as we move on to the next section, where we’ll share vital COPD prevention tips, especially for smokers.
Section 22: COPD Prevention Tips for Smokers
Preventing COPD begins with one clear message: Don’t start smoking, and if you already have, it’s crucial to quit as soon as possible.
- No Smoking: COPD is often referred to as a smoker’s disease. The most effective way to prevent it is to never start smoking. For those who have taken up the habit, remember, it’s never too late to quit.
- Immediate Benefits of Quitting: Research indicates that smokers can stabilize their lung function by quitting. Once you stop smoking, your lung health doesn’t continue to decline at the same rapid rate. In simpler terms, the deterioration plateaus, ensuring it doesn’t get worse at the same speed.
- Continued Smoking Worsens COPD: If smokers continue with the habit, their lung function will persistently decline. This can lead to a stage where COPD patients might require consistent oxygen support just to breathe normally.
For all smokers out there, whether you’ve started experiencing symptoms or not, the message is clear. Quitting smoking can significantly improve your lung health and reduce the risk of developing COPD. It’s a step towards a healthier future.
In our upcoming section, we’ll explore why even non-smokers are still at risk of developing COPD.
Section 23: Risks for Non-Smokers
While smoking is the leading cause of COPD, non-smokers are not entirely safe from the risks. Here’s why:
- Passive Smoking: Often overlooked, passive smokers can face severe health threats. These individuals inhale the unfiltered smoke emitted by active smokers, which can be even more harmful.
- Polluted Environments: It’s not just cigarette smoke that’s the concern. Exposure to exhaust from cars or other polluted air can also be a significant risk factor for COPD. So it’s essential to be mindful of the environment you’re in and limit exposure whenever possible.
- Biomass Exposure: Research from India has highlighted another potential risk. People exposed to biomass – the smoke produced from burning incense or animal feces – are also at risk of developing COPD.
In conclusion, while avoiding smoking is crucial, it’s equally important to understand the other environmental risks. COPD is not just a smoker’s disease; it can affect anyone exposed to harmful pollutants over a prolonged period. Whether you’re an active smoker, passive smoker, or someone frequently exposed to polluted environments, taking steps to limit these exposures can significantly reduce your risk.
In the next section, we’ll wrap up with a brief conclusion on the importance of understanding and preventing COPD.
Conclusion: Understanding and Preventing COPD
COPD, often associated with chronic smokers, is a complex and multifaceted respiratory disease. As we’ve explored, its effects are not limited to those who actively smoke. Passive smokers and even those exposed to certain environmental pollutants can find themselves at risk. The symptoms, while disruptive, can be managed with the right treatment and care.
However, prevention remains the most effective strategy. Whether it’s choosing not to smoke, avoiding secondhand smoke, or being conscious of our surroundings, these choices can significantly decrease the risk of developing COPD. For those already diagnosed, early detection, consistent treatment, and lifestyle changes can improve the quality of life.
Awareness is the first step. By understanding COPD, its causes, symptoms, and treatments, we can make informed decisions for our health and the well-being of those around us. It’s a collective effort to combat this disease, and every step taken towards a smoke-free and cleaner environment is a stride towards a healthier future.
If you require assistance for COPD
you can schedule an appointment
with Dr Nurul HERE



































